Herd Immunity Won’t Save Us
If we cannot stop COVID-19, can we even look forward to the moment in time when we all survive the disease and, presumably, will have immunity? The idea is tempting, but fatally flawed. Herd immunity can protect people, but it will not protect the population from a disease for which there is no vaccine.
Does this sound counterintuitive? Let’s take a quick look at what herd immunity is, how we achieve it, and what the outcome might be.
What is herd immunity?
When a contagious, fatal disease infiltrates a population, it leaves behind two things: corpses and survivors. From many diseases, including (we think) COVID-19, survivors are immune and cannot get infected again.
For an individual, immunity is protective. If I’m immune to COVID-19, I can go outside and not worry about getting sick. If everyone in the world is immune to COVID-19, I am still safe, even if I am not immune myself.
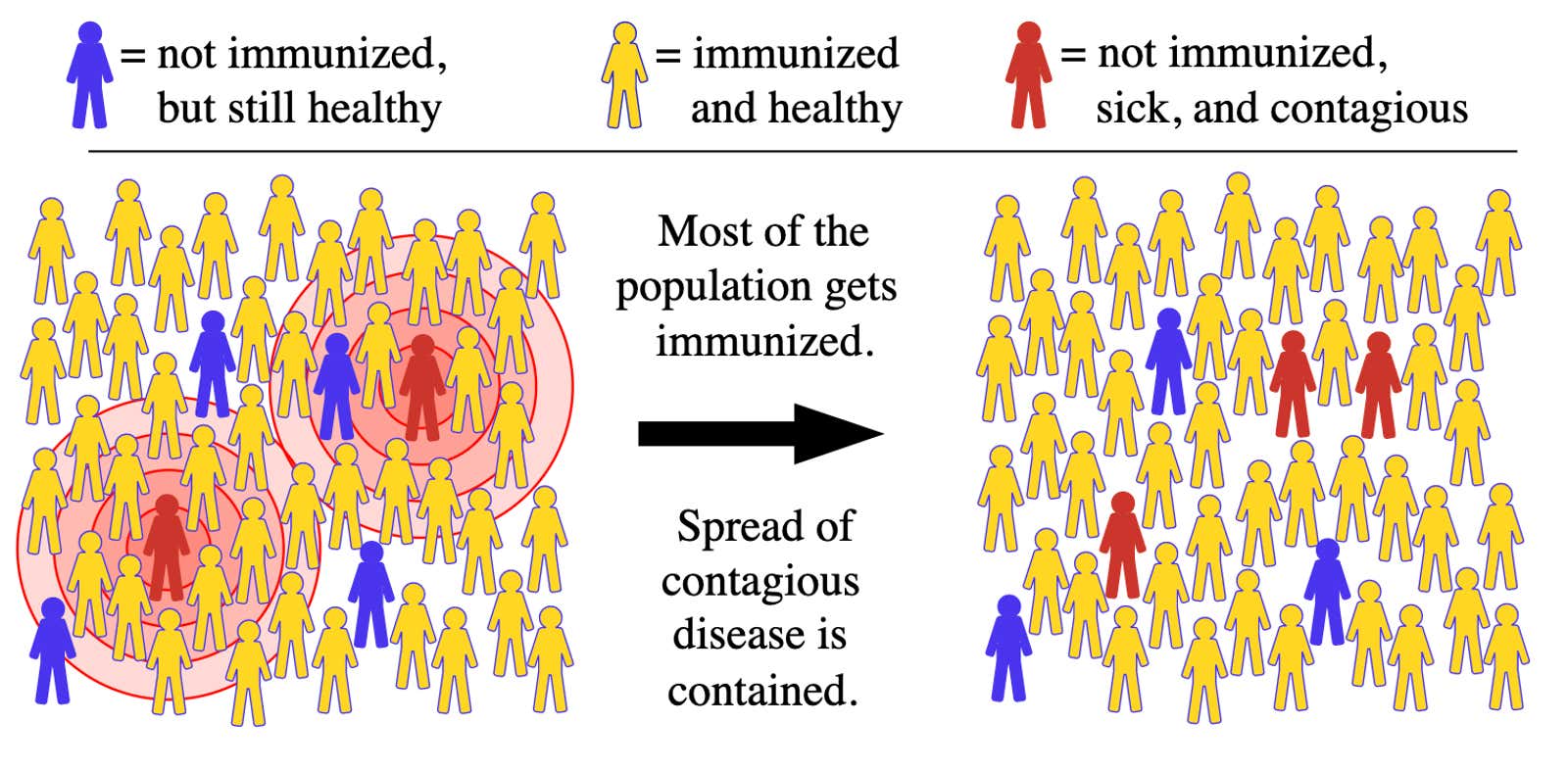
The idea of being immune to those around you is herd immunity. When we talk about vaccinations, that’s good. Let’s say 95% of your city’s residents have measles vaccinations. If a traveler comes to you with measles, there is not many opportunities for the disease to spread to another person. Vaccines protect most people in the city, and the few people who have not been vaccinated are protected by the simple fact that the disease has no way to get to them.
Herd immunity does not guarantee everyone will be safe, but it does mean that, on average, outbreaks pass quickly.
The percentage of people who need immunity to achieve herd immunity depends on the disease. Measles is highly contagious: every infected person can transmit it between 12 and 18 to other people in a population where no one is immune. COVID-19 does not spread easily. The exact number, or R 0 , is still being determined , although it is estimated to be in the range of 2 to 3. This means that we could achieve herd immunity if, say, 60% of the population were immune.
Sounds great, let’s go!
Not so fast. “All this talk of ‘Oh, once we get to herd immunity’ does not take into account the fact that herd immunity is achieved by getting everyone sick ,” says Ellie Murray , assistant professor of epidemiology at Boston University’s School of Public Health.
It may be possible to catch the coronavirus and not get very sick, and Murray notices this immediately, but she also pointed out that many infected people get very sick. Even those who survived may spend weeks in severe illness, may require hospital treatment, and may suffer from organ damage or other long-term consequences. We don’t even know what all these consequences could be, since the first people in history to have this disease recover in just a few months.
And people will die. In the United States, 2.7% of people with COVID-19 die from it. This number is still tentative and varies by country and age group, but if you apply it to the entire United States, you end up with millions of deaths.
Herd immunity protects us from measles because thanks to the vaccine we don’t need to get measles to get immunity. From a disease like COVID-19, which does not have a vaccine, the only way to get immunity is to get infected.
In short, “let’s all get sick” is not a solution to the problem of “how do we avoid everyone getting sick?”
But didn’t it work in Sweden?
Sweden is known to have adopted the herd immunity approach, which some American politicians call an effective strategy. But many more people died in Sweden than in neighboring countries , almost as many per capita as in the United States. and they also had a number of advantages that the United States does not. While some call this strategy a success, others might rightly say it looks like a ” disaster .”
The editor of the medical journal BMJ writes that Sweden may have been able to avoid the second wave, not because their herd immunity strategy worked, but perhaps because “the Swedes have followed the rules more obediently than in other countries – perhaps because they trust to the public. health officials understand what they need to do and why, and have avoided the confusion that worries the UK and other countries. ”
Sweden’s approach has not been to ignore the virus entirely. They banned gatherings of more than 50 people across the country. Workplaces and public transportation were needed to provide additional space for spacing. Sports events were held without spectators. People diagnosed with COVID were strongly discouraged from traveling.
Sweden also has a policy whereby people who do not work from home due to illness are paid 80% of their salary . It is of great importance for the probability that sick workers to stay at home. In the United States, many of us not only go to work sick for fear of losing income, but often have additional financial incentives to come to work, whether we are sick or not .
The herd immunity plan currently under discussion by the Trump administration (renamed “targeted protection”) does not appear to provide for paid sick leave or strict social distancing.
But if we were all sick, at least we would have immunity, right?
Okay, maybe. For some time. Remember, we don’t know how long immunity to COVID-19 will last. Based on what scientists know about other coronaviruses, immunity from COVID-19 could only last for a year or so .
Even if the survivors are found to have lifelong immunity, there is another problem. Most of the survivors will not be able to build a community for long. Travelers come to visit; babies are born. Before measles vaccination, measles epidemics occurred every few years . This is because it only took a few thousand babies to replenish the population susceptible enough for the outbreaks to recur. The numbers would be different with COVID-19, but the principle remains.
What if we only infect young, healthy people?
The first problem in this question is the word “we”. Who infects? Who signs people up for this experiment that will definitely have a fatality rate? This is not at all ethical.
But of course, let’s assume we’re okay with a bunch of people dying unnecessarily. (I, for the record, no.) Is there a way to infect only the people most likely to survive COVID-19? This is the idea behind proposals to reopen schools or to allow young people to return to work , keeping older people isolated.
The problem is, says Murray, that herd immunity does not apply to the population as a whole. This only matters in the network of contacts. If your grandfather mostly interacts with people in his nursing home, and none of them are immune to the virus, then one infected visitor is enough – you? – to provoke an outbreak throughout the building.
There is one more problem. The fact that we want to infect 60% (or whatever the herd immunity threshold) of the population does not mean that we can somehow control the outbreak and stop it when it reaches 60% . The epidemics are gaining momentum, and the epidemic, which has already infected more than half of the population, will continue. After all, if we are willing and able to stop the outbreak, why don’t we stop it at zero percent before it kills anyone?
And again it is “we”. It is completely unethical to send entire sections of the population to death, even if statistically we do not know who they are. Coercing or asking volunteers does not solve this problem, and the idea of creating a social structure based on immunity has a terrible and unfair history .
If we do establish herd immunity, it will cost a lot of human lives. It probably won’t last long. And it won’t be a way to win this test against the virus; this will be a confirmation that we have lost.
This post was originally published in April 2020 and was updated on October 14, 2020 with new mortality data and a section on what we learned from Sweden’s approach.